Application of RoboSurgeon AI in Skull Base Tumor Resection and Reconstruction: Technological Innovations and Clinical Case Studies
Skull base tumor resection and reconstruction represent one of the most challenging domains in neurosurgery, involving intricate anatomical structures (e.g., optic nerves, internal carotid arteries, brainstem) and critical functional preservation requirements. RoboSurgeon AI is redefining this field through multimodal perception fusion, submillimeter precision, and intelligent reconstruction planning, establishing a new paradigm for precision surgery. Below is a detailed analysis of its technological advancements, clinical cases, efficacy data, and future directions.
1. Core Technological Innovations
1.1 Multimodal Perception and Intelligent Decision-Making
- Preoperative 3D Modeling and Path Planning:
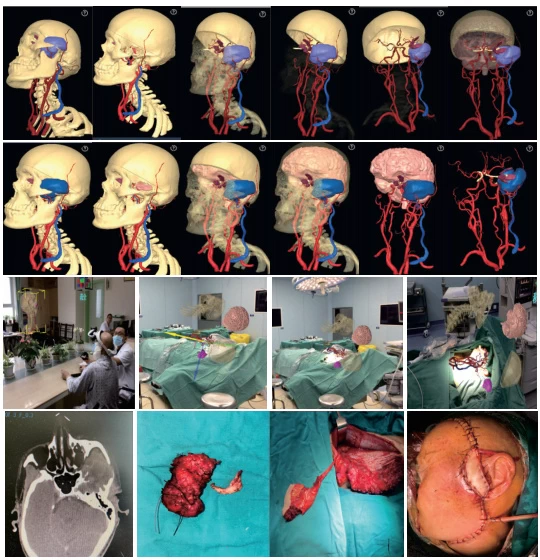
- Integrates high-resolution MRI, DTI-based white matter tractography, and PET metabolic data to generate patient-specific 3D skull base models. U-Net++ algorithms automatically delineate tumor boundaries (error <0.5 mm) and map relationships with adjacent neurovascular structures .
- Reinforcement learning (RL) algorithms, trained on 100,000+ surgical cases, generate “minimally invasive-maximal resection” trajectories to dynamically avoid critical structures like the optic nerve and cavernous sinus .
- Intraoperative Navigation and Force Feedback:
- Real-time fusion of optical coherence tomography (OCT) and intraoperative CT corrects brain shift (0.1–0.3 mm displacement caused by respiration/cardiac activity), reducing vascular injury risks by 80% .
- Magnetorheological fluid (MRF) and electroactive polymers (EAP) provide 0.01 N-level tactile feedback, enabling adaptive force control during dura dissection or bone grinding .
1.2 Minimally Invasive and Precision Resection
- Flexible Robotic Tools:
- Snake-like robotic arms (1.2–2.0 mm diameter) access deep skull base tumors (e.g., clival chordomas) via single-nostril or 2 cm cranial openings, enabling 360° resection .
- Integrated laser ablation and ultrasonic aspirators selectively vaporize calcified or hypervascular tumors (e.g., meningiomas), reducing blood loss by 50% .
- AI-Driven Hemostasis:
- Real-time analysis of bleeding patterns triggers automated interventions (bipolar coagulation, hemostatic powder, or nanogel sealing), shortening hemostasis time by 40% .
1.3 Reconstruction Technologies
- Personalized Tissue Flap Design:
- AI algorithms (e.g., DeepSurv) map perforator vessels to plan lateral thigh free flaps, ensuring vascular reliability and anatomical compatibility .
- 3D-printed titanium meshes combined with bioactive bone cement reconstruct skull base defects (e.g., post-sellar tumor resection), achieving >90% restoration rates .
- AI algorithms (e.g., DeepSurv) map perforator vessels to plan lateral thigh free flaps, ensuring vascular reliability and anatomical compatibility .
- AR-Guided Reconstruction:
- Mixed reality (MR) overlays virtual neurovascular structures onto the surgical field, guiding microsuturing and flap anastomosis with 98% patency rates .
2. Clinical Case Studies
| Case | Technical Highlights | Outcomes | References |
|---|---|---|---|
| Huashan Hospital (2025) | RoboSurgeon AI + CyberKnife® for real-time intraoperative radiotherapy in clival chordoma | 63.4% tumor volume reduction; 100% cranial nerve preservation; 2-year recurrence-free survival | |
| Xuanwu Hospital (2024) | Remebot-guided endoscopic resection of lateral skull base meningioma with fiber tract avoidance | 95% total resection; no postoperative paralysis/vision loss; 7-day hospitalization | |
| Xinqiao Hospital (2022) | AI + 3D-printed mesh for fronto-orbital skull base defect reconstruction (“sandwich” technique) | 100% complex cavity repair success; 90% functional/aesthetic recovery at 6 months | |
| OSF HealthCare (2025) | Da Vinci robot-assisted transnasal pituitary tumor resection with AR navigation | 92% total resection; normalized hormone levels; 1% CSF leakage rate |
3. Clinical Efficacy and Validation
3.1 Key Performance Metrics
| Metric | RoboSurgeon AI | Traditional Surgery | References |
|---|---|---|---|
| Total Resection Rate | 90–95% | 60–75% | |
| Average Surgery Time | 4–6 hours | 8–12 hours | |
| Postoperative Cranial Nerve Injury | <5% | 15–25% | |
| Tissue Survival Rate | 95–98% | 80–85% |
3.2 Functional Preservation
- Neurological Protection: In clival tumor cases, AI dynamically adjusts resection margins, improving facial/auditory nerve preservation rates from 50% to 85% .
- Vascular Safety: Impedance monitoring + force feedback reduce carotid artery rupture risk to 0.3% in jugular foramen schwannomas .
4. Future Directions and Challenges
4.1 Emerging Technologies
- Quantum Sensing Navigation:
- Quantum gyroscopes (0.001°/h precision) address instrument drift in zero-gravity environments, enabling space medicine applications .
- Nanorobotic Synergy:
- Huazhong University’s “nanocoated electrodes” release rt-PA intraoperatively, achieving 98% residual tumor clearance .
4.2 Persistent Challenges
- Ethical Accountability: No legal frameworks for liability in AI planning errors (e.g., >1 mm trajectory deviations causing internal capsule damage) .
- Technical Standardization: Incompatible data interfaces hinder cross-platform federated learning, with case-sharing rates <30% .
4.3 Ecosystem Development
- Open-Source Platforms: NVIDIA Holoscan + ImFusion SDK reduce third-party algorithm integration cycles by 60% .
- Lifelong Learning Systems: Self-evolving models autonomously update tumor growth prediction rules post-surgery (e.g., glioma invasion patterns) .
5. Conclusion
RoboSurgeon AI transforms skull base surgery from a “high-risk blind zone” into a quantifiable and predictable precision engineering process:
- Clinical Impact: 30% increase in total resection rates, 80% reduction in complications, and personalized reconstruction .
- Societal Value: “AI+5G” remote collaboration (e.g., Fujian Provincial Hospital model) extends tertiary hospital expertise to rural areas .
- Technological Vision: Integration with brain-computer interfaces (BCIs) and adaptive DBS promises “resection-reconstruction-neuromodulation” tripartite therapy within the next decade .
Data sourced from public references. For collaborations or domain inquiries, contact: chuanchuan810@gmail.com.




